Engineering Medicine: New Collaborations at the Boundaries of Disciplines
Engineering Medicine: New Collaborations
at the Boundaries of Disciplines
Imagine you’re one of the 16,000 people in the United States waiting for a liver transplant. Unlike those on the kidney transplant list, you cannot be treated with dialysis. Without a transplant your survival time is limited.
 |
Then a call comes: a liver is available. But there’s a catch: Because the deceased donor’s heart could not be kept beating during organ extraction — a so-called cardiac death donation — the liver has been deprived of oxygen for longer than is typical and may have deteriorated.
Do you wait and take your chances that you’ll receive a higher-quality liver? Or do you take the cardiac-death liver?
It’s a problem with no easy answer — and it’s an example of the type of problem that professors from Northwestern’s Feinberg School of Medicine and Robert R. McCormick School of Engineering and Applied Science are teaming up to solve. From studying transplant allocation to creating anatomy models with sensors to developing new kinds of drug-delivery methods and prosthetics, faculty in the two schools are calling, e-mailing, and traveling across Chicago to create connections that will ultimately improve all aspects of medicine. In 2010 more than 100 McCormick and Feinberg professors authored papers together, and new programs like mini-sabbaticals — where McCormick professors spend a quarter at Feinberg doing research—are inspiring new partnerships at all levels.
Health Care Engineering
Nowhere is the Feinberg-McCormick connection more apparent than in the Department of Industrial Engineering and Management Sciences, where faculty members such as Sanjay Mehrotra, PhD, and Gordon Hazen, PhD, are part of a new initiative called health care engineering. It aims to apply methods from statistics, computer science, and operations research to a variety of health care problems.
Take the liver decision problem — an issue Hazen, professor of industrial engineering and management sciences and an expert on health care decision analysis, has studied. In response to the long liver transplant waiting list, the United Network for Organ Sharing (UNOS), the national organ donation organization, has started encouraging organ procurers to consider more of what physicians refer to as “donor after cardiac-death” (DCD) livers.
“More donations has to be better, right?” Hazen asks. “But is it really better? What sense does it make to increase the number of low-quality organs procured if most patients should decline them and wait for a better organ?”
To explore the problem, Hazen created mathematical models that take into account what happens to patients on the liver transplant waiting list, including patient mortality and morbidity. Those models were used to predict what would happen if the number of DCD livers available for transplant increases or decreases. Hazen’s research showed that unless the liver patient is in critical need of a new liver, it doesn’t make sense to take a DCD liver.
 |
|
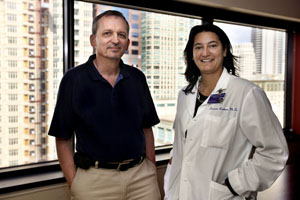
Gordon Hazen, PhD, professor of industrial engineering and management sciences, and Daniela Ladner, MD, assistant professor of surgery, collaborate on outcomes research for liver transplant recipients. |
Hazen collaborates with surgeons at the Northwestern University Transplant Outcomes Research Collaborative (NUTORC) on the University’s Chicago campus. Headed by Daniela Ladner, MD, assistant professor of surgery, the three-year-old initiative aims to connect transplant clinicians with cutting-edge researchers in seemingly disparate disciplines across campus.
“If you want to find better solutions, you have to collaborate,” Ladner says. “Collaborating with professors like Gordon Hazen and Sanjay Mehrotra helps us answer pertinent questions in the field of transplantation we couldn’t otherwise answer. It will ultimately help in our daily decision making for individual patients.”
While helping individual patients is, of course, a desirable outcome, the ultimate goal of the collaboration is to better inform and change transplant policy to reduce death rates of those on transplant waiting lists and improve decision making.
“I began working in this area because I was interested in decision analysis but also because I wanted to do research in something grounded in reality,” Hazen says. “Hopefully my models will help influence leaders and create change.”
Learning the Language of Medicine
While Ladner and her colleagues work with Hazen on risk prediction, they turn to Sanjay Mehrotra, professor of industrial engineering and management sciences and an optimization expert, for research on organ access and allocation throughout the United States. Over the past few years he has developed a half-dozen collaborations with Feinberg professors.
“I saw the value in this research,” he says. “None of us wants a systems failure that affects our health. Industrial engineers and operations researchers have helped develop a large analytical toolkit over the last 50 years. Historically, we could not use these tools for health care problems because the data were not as widely available. That’s changing. We can use our tools to better manage hospital systems, improve policy, and help make scientific discoveries.”
With NUTORC, Mehrotra and his graduate student Ashley Davis have studied kidney allocation. Nearly 90,000 people in the United States are waiting for kidney transplants. The country is divided into 11 regions managed by UNOS, and most kidneys are distributed within the same geographic zone in which they are donated. As a result, there are major regional inequalities in access to organs: a person in one state might get a kidney within a year, while someone in another state might wait up to four years. Many people die while waiting.
“It violates the ‘Final Rule,’ a government mandate about organ equity,” Ladner says. Mehrotra and Davis have created a new politically viable kidney distribution model to promote kidney sharing between regions.
“We’re using industrial engineering and operations research tools to fix this nationwide problem,” Mehrotra says. “Working with the transplant community, we are discovering structured, implementable policy changes that will be acceptable to both leaders and the population at large.”
In the course of researching the problem, Davis spends much of her time at NUTORC being mentored by Ladner and other clinicians. She essentially went through a mini–medical school boot camp to teach her how to think as both an engineer and a clinician.
“When you have people who understand both disciplines, you can open entirely new areas of research,” Ladner says.
Mehrotra also realized he had to learn the language of physicians after he became interested in the field a few years ago following several bad experiences in the health care system. So he took an undergraduate organic chemistry course.
“I was concerned I wouldn’t survive the quarter,” he says. “My lab partner was 30 years younger than I. But I took every single quiz, did every lab, and I survived. I learned the basic vocabulary.”
He cast his net wide, looking for collaborations, and word got around. He began working with Heron Rodriguez, MD, a vascular surgeon, and Debra DaRosa, PhD, vice chair of education, department of surgery, on scheduling surgical resident rotations. He began a project with David Liebovitz, MD, chief medical informatics officer for the Northwestern Medical Faculty Foundation, considering how to best restrict unauthorized access to patient records. He is working with Jeffrey J. Goldberger, MD, a cardiologist, and George Chiampas, DO, an emergency medical physician on better risk assessment of patients with cardiac conditions and on systems solutions that address the vexing problem of sudden death due to cardiac arrest, which kills nearly 400,000 people every year in the United States.
“Given the number of problems that need data-driven engineering solutions, we can engage students at every level,” Mehrotra says. "Undergraduate students get real-world experience when working on their projects, and the collaborations are leading to new sources of funding for graduate students to work on practical problems while developing new methodologies.”
Health Care Engineering beyond Graduation
One of those graduate students was Jonathan Turner. A student of Mehrotra who received his PhD in May, Turner spent six months at Northwestern Memorial Hospital shadowing surgery residents and collecting data for what would ultimately become the subject of his dissertation: improving surgery education.
Surgeons at the hospital noticed that surgical residents gained varying amounts of experience. Often, the first time they met a patient was in the operating room — hardly a typical experience for a surgeon.
“Residents spend only one or two months on vascular surgery rotation,” Turner says. “The time between diagnosis and surgery is often three weeks. Probability models showed the vascular surgeons that without some logistical changes, the odds that a resident would be able to see the same patient for both diagnosis and surgery were very small.”
As a result of these findings, Turner created scheduling software that allows surgeons to match residents with patients. That means the resident is able to spend more time with the patient from diagnosis to surgery to follow up and results in a more realistic and valuable educational experience. Turner’s software has been piloted at the hospital and an upgraded version is planned for the future.
“The software allows residents to have a sense of patient ownership they didn’t have before,” Turner says. “There is a story behind each patient. As care gets more and more fragmented, those stories get harder and harder to see. We can help doctors meet that challenge through scheduling assistance.”
Feinberg and Northwestern Memorial Hospital were so impressed with Turner’s work that they hired him as the hospital’s first health care engineer manager for quality and innovation.
“Our research goal is to leverage health delivery science and raise the value of health care delivery by improving process quality and patient outcomes while reducing cost,” he says.
Turner’s first projects involve finding ways to reduce handoffs of patients from doctor to doctor and reorganizing nurses’ charts to avoid redundancies. Mark Williams, MD, professor and chief of hospital medicine, and Turner, working with Mehrotra, have also proposed a Northwestern University Center for Value and Innovation in Health Care Delivery, which would further encourage Feinberg-McCormick connections.
“I want to be a facilitator,” Turner says. “I want to say, ‘Here is a problem, and here is the best person in McCormick to work on that.’ I can distinguish whether a project might make a good dissertation or an ideal undergraduate assignment. I plan to make McCormick faculty aware of good research projects that are outside my skill set.”
An added benefit is that the work of Turner and others isn’t just advancing the field of medicine, it’s also advancing the state of industrial engineering and operations research. “My ultimate hope is that these new methodologies will solve problems beyond health care,” Mehrotra says.
Bio-inspired Results
McCormick connections with Feinberg go beyond operations research. Many biomedical and mechanical engineering professors have close relationships with physicians, surgeons, and rehabilitation specialists at the medical school. Dean Ho, for example, is using biomaterials for next-generation medicines.
Ho, associate professor of biomedical and mechanical engineering, is working on a project with Patrick McCarthy, MD, director of the Bluhm Cardiovascular Institute and chief of cardiac surgery, and Sunjay Kaushal, MD, PhD, assistant professor of surgery, to create a patch that can help the heart heal after surgery. (Ho met McCarthy through another McCormick-Feinberg connection: the course NUvention: Medical Innovation, in which students from across Northwestern create and market medical devices.) The patch, which looks like plastic wrap and is made of Parylene, attaches directly to the heart and can release anti-inflammatory, antiscarring, and anti-arrhythmia agents and pain medication for defined periods of time. When Ho and his group first developed the film employed in the patch, they brought it to McCarthy and asked him a series of questions: How thick do you want it? Would this be easy to handle in the operating room? How difficult would it be to affix to the heart?
“It’s great to work with someone who is so involved in the medicine-engineering interface,” Ho says. “Having a surgeon standing right there really helped accelerate the development of the technology.”
Ho also recently started a project with Charles Clevenger, MD, PhD, professor of pathology, to use nanodiamonds to deliver emerging therapeutics for breast cancer. Nanodiamonds have a carbon structure similar to the diamonds found in jewelry but are much smaller: hundreds of thousands of these nanodiamonds could fit on the head of a pin. Ho has used nanodiamonds for other cancer treatments such as chemotherapy. They are ideal for carrying chemotherapy through the body because they shield the drug from normal cells and don’t cause inflammation. Ho hopes the nanodiamonds will help stabilize the new therapeutics and make them last longer.
“The diamond keeps the drug in the tumor longer,” he says. “We’re pretty excited.”
In a field like Ho’s, connections like these are critical.
“It’s important to have a proactive dialogue between the engineer and the end user, the clinician,” he says. “Interacting with Feinberg professors gives us key details on how to improve the design. Ultimately it’s what is needed to push translational medicine forward.”
Feinberg connections with McCormick extend to education in biomedical engineering as well. For the past several years undergraduates have worked with John Vozenilek, MD, associate professor of emergency medicine and director of the Center for Simulation Technology and Immersive Learning, to create lifelike simulation models for health care education. Vozenilek has worked with students in several senior design courses to create models for the developing world. Their projects have included a wireless EMG sensor and a placenta model.
“Engineering students have consistently created devices for developing countries that don’t exist in the market,” he says. “This gives us an opportunity to think creatively about what we can do that is inexpensive and durable. And frankly, we’re having a lot of fun doing it. The students are really engaged and excited. They provide new perspectives, which I really appreciate.”
Medical Education and Electrical Engineering
To create simulation models for education and testing, McCormick and Feinberg have also looked to other disciplines. Take the collaboration between Carla Pugh, MD, PhD, and Chang Liu. Pugh, an associate professor of surgery, knows models: as director of the Center for Advanced Surgical Education, she has made more than 20 simulation models over the past 15 years that have been used to teach medical students how to do everything from pelvic exams to laparoscopic surgery.
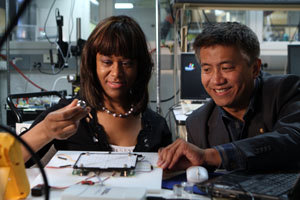 |
| Carla Pugh, MD, PhD, associate professor of surgery, and Chang Liu, professor of electrical engineering and computer science, have teamed up to create a state-of-the-art simulation model that will test how well physicians perform breast exams. |
“I build anything I see a need for,” she says.
Pugh knew that the direct-force sensors she used in her models were no longer satisfactory. If she had better sensors, she could get much better data on how well doctors are performing diagnostic exams that require touch. Enter Chang Liu, professor of electrical engineering and computer science and of mechanical engineering. He knows sensors: using micro- and nanofabrication technology, Liu creates innovative artificial hair cells that can sense force from several directions.
Now the two have teamed up to create a state-of-the-art model that will test how well physicians perform breast exams.
“It could change the way we define competency for hands-on clinical performance,” Pugh says. “To be able to quantify something like touch is a worldwide goal.”
Palpation tests like breast exams involve many fingers that do complex maneuvering, so Liu and his graduate students began building a sensor plate that could measure multidirectional and sliding forces from five different fingers.
“It’s an open field,” Liu says. “We’re in no man’s land. That is where raw creativity and scientific discipline come in.”
Pugh and Liu have begun building an array of sensors that can sense sliding and complex motions for a single finger, and they are working to expand the capability to several fingers.
“For five fingers we need something fresh,” Liu says. “We’re trying multiple approaches.”
When the model is finished, Pugh will take it for testing at medical conventions. There she can gather data on how doctors usually move their fingers during exams. She hopes to expand the technology to other tests, and Liu hopes his new approach to sensors could be used outside the medical field. Either way, their collaboration is sure to push the state of the art.
“Collaborating should be the norm,” Pugh says. “I think that’s the wave of the future. We can no longer work in academic silos. Innovation comes from bridging two disciplines together. This is where it happens.”
Collaborating for Rehabilitation
McCormick-Feinberg collaborations have had a host of successes in physical rehabilitation as well. A few years ago, Ed Colgate, professor of mechanical engineering and the Allen K. and Johnnie Cordell Breed Senior Professor of Design, and Michael Peshkin, professor of mechanical engineering, teamed up with Todd Kuiken, MD, PhD, professor of physical medicine and rehabilitation at Feinberg, to create a prosthetic arm that reads nerve impulses and provides the user with touch feedback.
Using an innovative procedure called targeted reinnervation surgery, Kuiken grafted the nerve endings that once went into an amputee’s limb onto the amputee’s pectoral muscle. Once the nerve endings grew into their new location, Kuiken and his team could use sensors to read the impulses of the nerve to move a prosthetic limb. Unexpectedly, these nerve endings were also able to receive input, meaning that new prosthetic devices could actually provide touch sensation to the user as a real limb would. Colgate and Peshkin used their research in haptics — tactile feedback technology that uses touch as an interface — to give the arm “touch feedback” capabilities.
The connection between biomedical engineering and physical rehabilitation has also helped biomedical engineering associate professor Eric Perreault, PhD, and assistant professors Wendy Murray, PhD, and Matthew Tresch, PhD, — all of whom have joint appointments in physical medicine and rehabilitation. Murray, for example, uses computer simulation techniques and experimental methods to investigate how humans move and control their arms and hands. Tresch used a model of the muscles in a frog’s hind leg to perform a computational analysis showing that researchers could control the limb using muscles groups just about as well as by controlling individual muscles.
With all these successes, there is still room for growth. Minisabbaticals are allowing more McCormick professors to spend a quarter conducting research at Feinberg, and Feinberg professors have come up to the Evanston campus to give seminars. This past spring Nathaniel Soper, MD, the Loyal and Edith Davis Professor and chair of surgery at Feinberg, visited with McCormick professors and students and discussed how to encourage more medicine-engineering connections. Professors from both schools were eager to build on the expertise of others and pave more roads between the disciplines.
“We need to figure out how to make this work between us,” Soper said. “We were meant to take care of humans, and we can do it better if we work together.”
– Article courtesy of Robert R. McCormick School of Engineering and Applied Science. Written by Emily Ayshford